Understanding Sleep Challenges for Seniors
As we grow older, changes in our body’s natural rhythms and health can make a full night’s sleep harder to achieve. While most adults need around seven to eight hours of sleep, many older adults find themselves waking frequently during the night or rising too early in the morning.

Common sleep problems in seniors include insomnia, frequent night time awakenings, early morning waking, and non-restorative sleep. Disorders such as sleep apnea and restless legs syndrome are also more prevalent in older adults.
Several factors contribute to these disturbances. Age-related changes in the sleep cycle reduce deep, restorative sleep. Pain, medications, stress, depression, and night time urination also play roles. Environmental conditions like noise, temperature, and lighting can make it even harder to stay asleep.
The health implications of poor sleep are significant. Chronic sleep deprivation has been linked to memory decline, weakened immune function, higher risk of falls, and even cardiovascular problems. For seniors, prioritizing sleep is not a luxury, it is a cornerstone of healthy aging.
Why Do the Elderly Have Trouble Sleeping?
Aging and sleep patterns:
With age our circadian rhythm, the internal body clock that regulates sleep and wake cycles, tends to shift earlier. Many seniors feel sleepy sooner in the evening and wake earlier in the morning. Additionally, the proportion of deep (slow-wave) sleep decreases, while lighter sleep stages increase, making it easier to wake up from minor disturbances.

Medical factors:
Chronic conditions such as arthritis, heart disease, diabetes, or respiratory problems can cause discomfort or pain that interrupts sleep. Nocturia (frequent urination) and sleep apnea are particularly common culprits.
Medication effects:
Many prescriptions , including corticosteroids, certain antidepressants, beta blockers, or diuretics, can alter sleep quality or timing. Reviewing medications with a healthcare provider can reveal hidden causes of insomnia.
Psychological influences:
Depression, anxiety, and loneliness can interfere with the ability to relax and fall asleep. Emotional stressors such as loss, caregiving, or major life changes often worsen sleep problems.
Lifestyle and environmental factors:
Irregular schedules, long daytime naps, limited exposure to sunlight, caffeine or alcohol use, and evening screen time all disrupt the body’s natural sleep signals. Simple behavioral adjustments often make a major difference.
The Best Sleep Aids for Older Adults
Before turning to medication, it’s wise to explore safer, natural options and behavioral strategies. Below is an overview of both non-prescription aids and supplements that may support restful sleep, along with guidance on when medical treatment is warranted.
When considering supplements for sleep, it’s important to understand that none are magic cures. The evidence is mixed, especially in older populations. Supplements may help as part of a broader sleep plan, but they should be used carefully, with awareness of interactions, dose, and underlying health conditions.
Here are some of the more studied supplements, what the evidence suggests, and safety considerations:
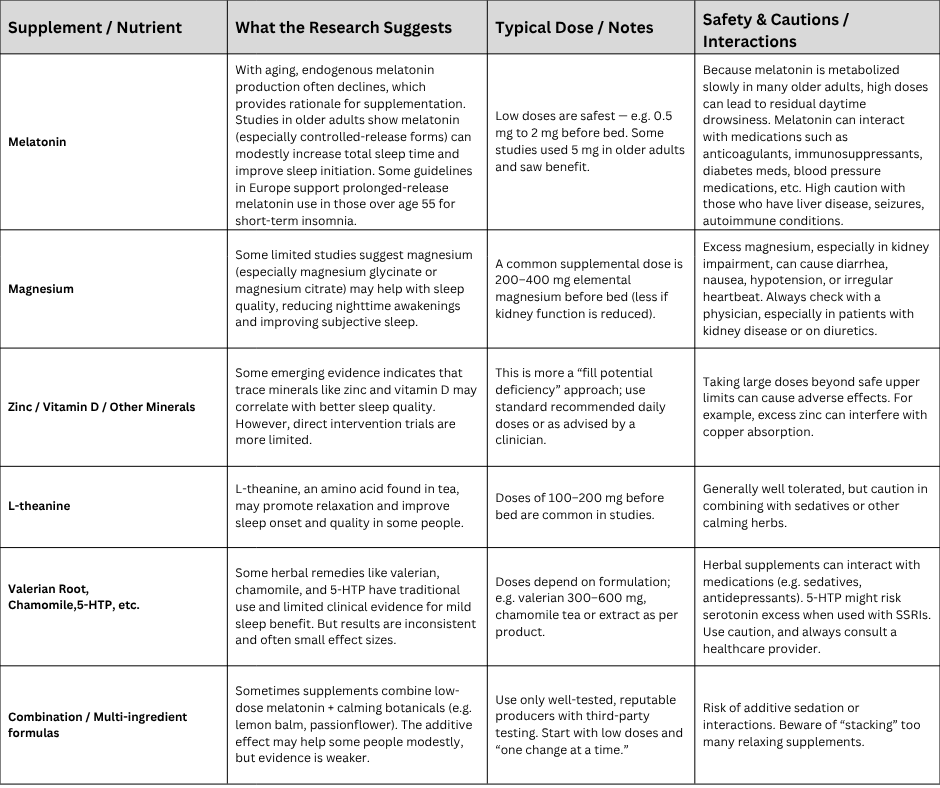
Best practices / tips when using supplements:
- Always start with the lowest effective dose; avoid “more is better.”
- Use for short-to-moderate durations (e.g. several weeks), not indefinitely, unless guided by a clinician.
- Monitor for side effects (daytime drowsiness, dizziness, digestive upset).
- Always review with the person’s physician or pharmacist, especially in older adults who often take multiple medications.
- Supplements are adjuncts, not replacements for good sleep habits and addressing root causes.
Non-Prescription & Natural Sleep Aids

- Melatonin:
Natural melatonin production declines with age. Low doses (0.5 – 2 mg) about 30–60 minutes before bedtime can help regulate the body clock. Prolonged-release forms may benefit those who wake frequently. - Magnesium:
Supports muscle relaxation and nerve function. Magnesium glycinate or citrate (200–400 mg nightly) may ease nighttime awakenings, but should be used cautiously in those with kidney issues. - L-theanine:
An amino acid from green tea that promotes calm without sedation. 100–200 mg before bed may reduce mental tension. - Herbal options:
Valerian root, chamomile, lemon balm, or passionflower are traditional relaxants with modest evidence for improving sleep onset. - Zinc and Vitamin D:
Deficiencies in these nutrients have been linked to poor sleep quality. Ensuring adequate intake through diet or supplementation can help.
Prescription Medications
For persistent insomnia unresponsive to lifestyle changes, a physician may recommend medications such as:
- Low-dose doxepin or melatonin receptor agonists, which are generally safer for seniors.
- Dual orexin receptor antagonists (like suvorexant) can also be effective, though cost and side effects vary.
Traditional sleeping pills (benzodiazepines or “Z-drugs”) are usually avoided in older adults due to increased risk of falls, confusion, and dependence.
Pros and Cons
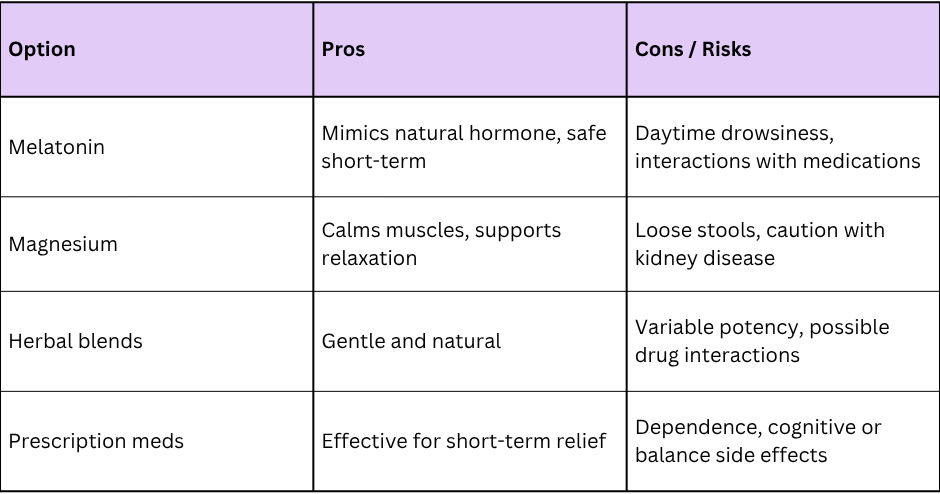
Always consult a healthcare professional before starting any supplement or medication, especially if you take other prescriptions.
Effective Strategies to Improve Sleep in Seniors
While supplements may help, the foundation of healthy sleep lies in daily habits and routines.
Maintain a Consistent Schedule
Going to bed and waking up at the same times each day helps regulate your internal clock. Even on weekends, stick to a regular rhythm.
Nutrition and Diet
- Limit caffeine and alcohol, especially after mid-afternoon.
- Eat lighter dinners and avoid heavy or spicy meals close to bedtime.
- A small snack with tryptophan-rich foods (like yogurt, banana, or oatmeal) may promote relaxation.
Physical Activity
Regular movement enhances sleep quality. Gentle exercises such as walking, swimming, or tai chi help regulate hormones and reduce stress. Avoid intense workouts within three hours of bedtime.

Mindfulness and Relaxation
Relaxation techniques can calm the mind before bed:
- Deep breathing or progressive muscle relaxation
- Guided meditation or prayer
- Listening to calming music
- Reading or light stretching
Chronic stress elevates cortisol, which can delay sleep onset. Managing tension during the day supports better nights.
Creating a Sleep-Friendly Environment
Your bedroom environment can make or break a good night’s rest.
Optimize Lighting and Temperature
Keep your room cool (around 65–68 °F / 18–20 °C) and dark. Blackout curtains or eye masks help block light, while dim night-lights provide safety for bathroom trips.
Reduce Noise
Use earplugs, white noise machines, or soothing nature sounds to mask environmental noise.
Choose Comfortable Bedding
Invest in a supportive mattress and pillows suited to your sleep position. Soft, breathable bedding and loose sleepwear can prevent overheating or irritation.
Go Tech-Free Before Bed
Screens emit blue light that suppresses melatonin. Turn off TVs, tablets, and phones at least an hour before sleep. Instead, engage in a quiet activity that signals your body it’s time to wind down.
Establish a Calming Routine
Create a simple nightly ritual — dim lights, gentle stretches, warm bath, or herbal tea. Repetition conditions the mind to associate these cues with rest.
Professional Guidance and Resources
If sleep problems persist despite healthy habits, professional help is essential.
When to Consult a Sleep Specialist
- Difficulty sleeping for more than three nights per week for over a month
- Excessive daytime fatigue or falling asleep unintentionally
- Loud snoring, choking, or gasping during sleep (possible sleep apnea)
- Restless legs or jerking movements at night
A sleep specialist can perform tests to identify underlying disorders and recommend individualized treatment.

The Importance of Health Check-ups
Regular medical check ups and reviews ensure that medications, pain conditions, or chronic diseases are not undermining sleep. Adjusting medication timing or dosage often makes a big difference.
Tips for Caregivers
Caregivers can support seniors by encouraging consistent schedules, limiting stimulants, and promoting a peaceful environment. Keeping a sleep diary can help track improvements and identify triggers.
Trusted Resources for Information
National Institute on Aging (NIA): A division of the US Department of Health and provides health information informed by research and reviewed by experts to help learn about healthy aging.
Sleep Foundation: Features expert written content on sleep hygiene and other related topics, including the one on Mastering Sleep Hygiene
NHS (National health Service): In UK and provides extensive information on sleep disorders and problems, including resources on insomnia, narcolepsy, and advice on seeking medical help through resources like GP support or online helpline.
Age UK: Offers advice and information on sleeping well in later life, including details on the connection between sleep and brain health, and can provide information on support services.
Final Thoughts
For older adults, quality sleep is one of the most powerful tools for maintaining vitality, memory, and mood. By combining healthy routines, a calm environment, and targeted nutritional support, restful nights are possible at any age.
Before beginning any supplement or medication, always consult your healthcare provider and but don’t underestimate the healing power of small daily habits and a peaceful bedtime routine.
